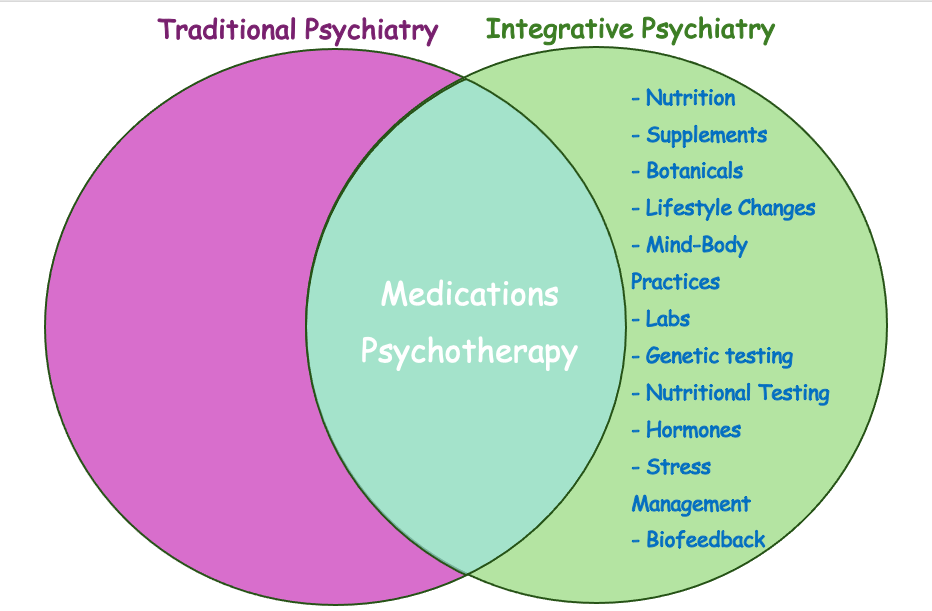
When most people think of psychiatry, they picture a quick check-in with a prescribing doctor—answering yes-or-no questions and leaving the office within 15–20 minutes. From my experience as a provider who once worked in this fast-paced model, many clients feel rushed and only superficially helped. While this conventional model of psychiatry has helped countless people, it is not sufficient for everyone. For a large subgroup of individuals, mental health needs to be addressed in a fundamentally different way. What I see every day is a growing need for care that treats the whole person—mind, body, and lifestyle—not just the diagnosis. Many of my patients do not get better with medications alone. This is exactly where integrative psychiatry comes in.

What Is Conventional Psychiatry?
Conventional (or “traditional”) psychiatry focuses on diagnosing mental health conditions and treating them primarily with medications and psychotherapy. Most appointments are 15–20 minutes long—barely enough for medication management, let alone meaningful psychotherapy. In traditional psychiatry, we typically see:
- Assessment: Symptom checklists, brief histories, and standardized diagnostic criteria such as the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) that psychiatrists use to match symptoms with a diagnosis
- Treatment tools: Psychiatric medications, referrals for therapy, and sometimes hospitalization.
- Strengths: Decades of research on medications, clear evidence-based protocols, and effective interventions for acute states.
This approach can absolutely be lifesaving—I’ve seen it work wonders both inpatient and outpatient. But for many people—especially those with chronic stress, mild to moderate symptoms, or complex conditions—the conventional model feels limited and impersonal. It doesn’t look deeply enough at all aspects of the problem.
What Is Integrative Psychiatry?
Integrative psychiatry blends the best of conventional psychiatry with evidence-based complementary and lifestyle approaches. It’s a “whole-person” framework that looks beyond symptom relief to the root contributors to mental health. Patients receive not just a diagnosis and a prescription but also a roadmap for long-term resilience and well-being.
Key features of integrative psychiatry include:
- Comprehensive evaluation: In addition to a psychiatric interview, your clinician may look at nutrition, sleep, movement, stress levels, trauma history, social support, hormone status, lab results, and even genetic and nutritional testing.
- Expanded toolkit: Medications when needed plus targeted supplements, nutritional strategies, movement, stress-reduction practices, psychotherapy, and mind–body therapies such as breathwork or biofeedback.
- Collaborative care: In my integrative psychiatry practice, I provide clear explanations of each treatment option—its benefits, limitations, and potential side effects—so patients understand the reasoning behind recommendations. This education allows them to take part in mutual decision-making, rather than feeling left out of their own care.
Why Integrative Psychiatry Is Different
Integrative psychiatry recognizes that mental health is inseparable from physical health, relationships, and environment. It goes beyond symptom management to address nutrition, sleep, hormones, inflammation, stress, and meaning. By weaving together medication management with mind–body practices, nutritional guidance, and psychotherapy, integrative psychiatry creates a far more personalized and empowering path to wellness.
Many people come to integrative psychiatry after feeling unheard or stuck in the conventional model. Others start here from the beginning because they want prevention, resilience, and a values-aligned approach. Whatever the reason, the goal of integrative psychiatry is the same: to treat the whole person, not just the diagnosis.
The Bottom Line
Conventional psychiatry saves lives, especially in crises. But for those whose needs extend beyond a prescription, integrative psychiatry offers a comprehensive, evidence-based, and collaborative way to heal. By bringing together the science of modern psychiatry with nutrition, lifestyle, and mind–body practices, integrative psychiatry empowers patients to recover, grow, and thrive.
The Main Differences at a Glance
| Aspect | Conventional Psychiatry | Integrative Psychiatry |
| Focus | Symptom management | Root causes + symptom relief |
| Tools | Medications, psychotherapy | Medications, psychotherapy, lifestyle, nutrition, supplements, mind–body practices |
| Evaluation | Standard psychiatric assessment | Expanded assessment (labs, genetic testing, diet & nutritional testing, sleep, hormones, inflammation) |
| Patient Role | Passive, compliance-oriented | Active, collaborative |
Leave a comment